Published: 04/30/2021
In an increasingly interconnected world, the next pandemic is not 100 years away. Here’s what scientists are worried about and how we can prepare.
Written by Deni Ellis Béchard.
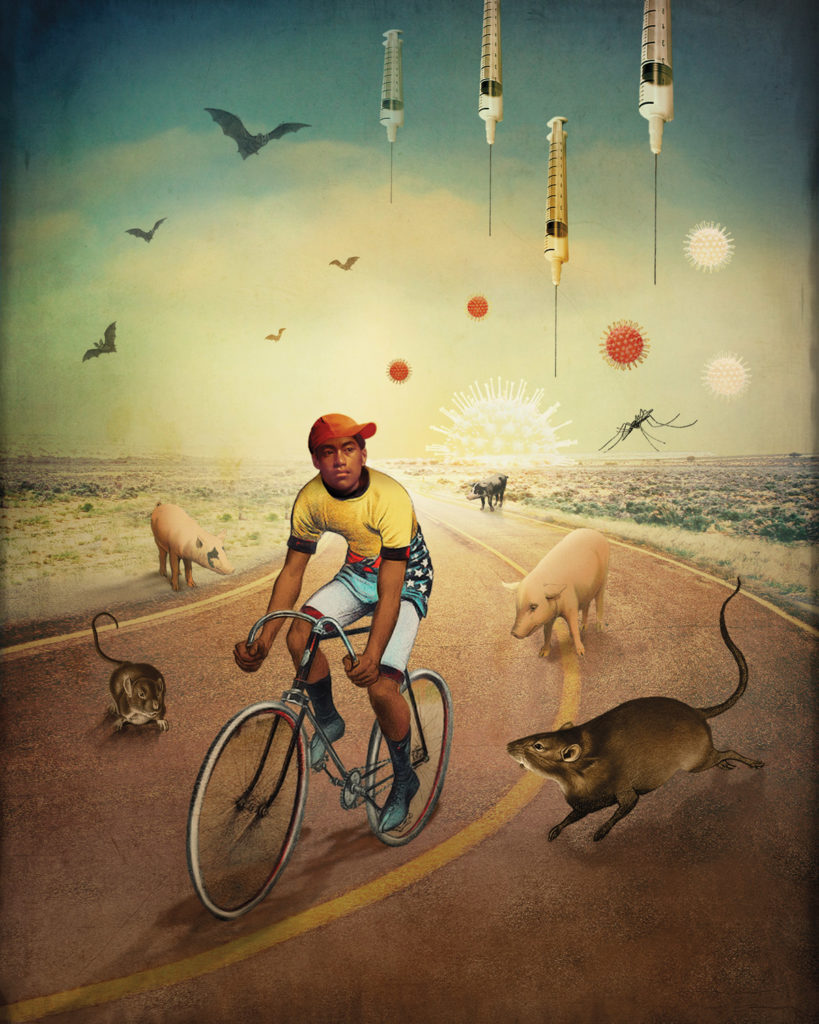
Illustrations by Catrin Welz-Stein.
Maria Van Kerkhove crossed the yard to the bedroom window of her sons, then 9 and 1, to wave to them. For two months—“the worst of my life,” she recalls—she saw them and her husband only through glass. The novel coronavirus was spreading in Geneva, Switzerland, where Van Kerkhove, MS ’01, is the World Health Organization’s technical lead for COVID-19 response, and too little was known about the disease for her to risk exposing her family. “A lot of people have asked me if that was an exaggeration,” she says. “You have to remember that time and the uncertainty in it.”
She, like millions of others, has since learned much about SARS-CoV-2, the virus that causes COVID-19. And yet a question remains as to how the virus first infected humans—an important one for Van Kerkhove, an epidemiologist who also heads the WHO’s unit for emerging diseases and zoonoses (animal diseases that have spilled over into human populations). Understanding the path each zoonotic disease takes to reach humans is crucial for developing strategies to prevent, detect and respond to future outbreaks. “By some estimates, 70 to 80 percent of emerging and reemerging pathogens are zoonotic,” she says, “so we always expected that the next one—Disease X—could be a zoonotic pathogen.” But though SARS-CoV-2 originated in bats, the story isn’t simple, and its journey to humans may have taken years. For instance, the MERS (Middle East respiratory syndrome) coronavirus, which was transmitted from bats to camels to humans, was first documented in 2012, but analysis of stored camel blood has revealed the presence of MERS antibodies as far back as 1983. “This means that MERS coronavirus was circulating among dromedary camels for almost 40 years—for at least that long,” Van Kerkhove says. In January 2021, a WHO team traveled to Wuhan, China, and examined the Huanan Seafood Market, where the COVID-19 outbreak was initially thought to have begun. They determined that the virus could have hitched a ride with a number of species sold there: rabbits, civets, ferret badgers, raccoon dogs, pangolins—some of which, though wildlife, are raised for slaughter in other provinces. The virus could have been circulating in animals for years, mutating and becoming better adapted to humans, before the urban density of Wuhan—a city of 11 million—provided the perfect setting for a massive outbreak. “The Huanan market itself was an amplification event,” Van Kerkhove says. “It wasn’t the start of the pandemic.”
News outlets have called COVID-19“a once-in-a-century pandemic”—as if, when it’s over, the human race can indulge in a 100-year-long unmasked sigh of relief. But today’s earth is not that of 1918, when we last saw an outbreak this disruptive. Since then, the world population has quadrupled, increasing by 6 billion, in lockstep with livestock breeding, the destruction of forests and global warming. Not for the distant future but for this world, as it is now, COVID-19 provides a cautionary tale—of transmission between wildlife and humans, of densely packed urban areas, of a globe as wound up as a ball of yarn but with highways and flight paths. This, though, is a tangled tale: In nature, all is connected, and in ways that humans have only begun to imagine.
In the Beginning
Wrath of gods or evil spirits, epidemics are mentioned often enough in ancient texts as to count among life’s inevitabilities. While some civilizations may have understood the source of infection—hence cultural prohibitions against eating certain animals—the full extent of zoonoses was unknown. The bubonic plague originated in gerbils; genetic studies have traced smallpox back millennia to rodents, and measles to cattle. Well into the 19th century, diseases were often transmitted from animals to humans via milk until Louis Pasteur turned the page on that era with his eponymous technique in 1862. He later devised vaccines for two zoonotic bêtes noires, anthrax and rabies. Today, scientists continue to refine their understanding of zoonoses, increasingly advocating for surveillance of hot spots.
Among the most monitored viruses is the one we know best: the flu. Specifically, the avian flu, passed from migrating birds to poultry. In 2009, Van Kerkhove finished her PhD on the avian flu and shortly afterward became a WHO consultant, when that year’s influenza pandemic began. Whereas the avian flu virus is poorly adapted to humans (difficult for us to transmit, though often causing fatal illness), pigs are susceptible to both human and avian flus, providing a crucible in which a virus can mutate. The best-known virus to emerge in this fashion was the 1918 flu, which may have claimed 3 to 5 percent of the world’s population—50 to 100 million people. The 2009 influenza, dubbed the swine flu, was another interspecies alchemy. Since then, avian flu has been transmitted to humans many times, often directly from birds. “It just keeps going,” Van Kerkhove says. “You have spillover events and then a small outbreak, but it hasn’t taken off.”
Stephen Luby, a professor of medicine and a senior fellow at the Woods Institute for the Environment, has also researched avian flu outbreaks. “Had we had this conversation 14 months ago,” he said in January, “we probably would have spent it all on influenza and not said a word about the coronaviruses, because communicable disease epidemiologists are constantly looking back to 1918 and saying, ‘It could happen again.’ ”
Whereas COVID-19 having already claimed nearly 3 million lives has a 1 to 2 percent fatality rate, Nipah’s can be as high as 75 percent, worse than the Black Death’s.
During his eight years in Bangladesh with the Centers for Disease Control and Prevention, Luby discovered that an obstacle to decreasing avian flu outbreaks lay in people’s relationship with their poultry. “Eighty-five percent of the rural population in Bangladesh raise chickens,” he says. “The return on investment is on the order of 300 percent. These are low-income settings, so you want to raise poultry, and the cheap way to do that is to have them run around your hut. Then, at night, people usually bring them into the home and, most commonly, put them under the bed.” Though such frequent contact could create a virus adapted to humans, people are reluctant to forgo economic benefits. “We’re arguing from the perspective of pandemics, which are low-probability, high-consequence events,” Luby says. “The issue here isn’t about education and knowledge. It’s really about incentives.”
However, Luby has seen success mitigating outbreaks with a virus that few know by name but that anyone who’s seen the 2011 film Contagion knows in spirit: Nipah. While it doesn’t actually melt your brain, as depicted during the autopsy of Gwyneth Paltrow’s character, initial symptoms include fever, coughing and vomiting, followed by seizures, coma and often-fatal encephalitis. Today, Nipah is among the world’s most surveilled viruses. Whereas COVID-19—having already claimed nearly 3 million lives—has a 1 to 2 percent fatality rate, Nipah’s can be as high as 75 percent, worse than the Black Death’s, which wiped out a third of Europe’s population during the late Middle Ages.
Luby recalls leaving a CDC conference on Nipah earlier in his career, shaking his head and thinking, “That is one bad virus. Glad I don’t have to work on that.” A few years later, in Bangladesh, he was studying Nipah outbreaks and prevention. Fortunately, whereas SARS-CoV-2 is airborne—diffused during normal breathing and able to linger in the air—Nipah is transmitted via large aerosolized droplets from coughing that don’t carry far. “We’ve had dozens and dozens of spillovers,” Luby says, “but the virus has never been efficient enough in person-to-person transmission to sustain ongoing transmission. But we worry that the virus has changed just as we’re watching SARS-CoV-2 change now.”
Though COVID-19 is to Nipah what hand grenades are to heavy artillery, they both—like rabies and Ebola—originated in bats. In Nipah’s case, large fruit bats savor date palm sap, which Bangladeshis collect similarly to maple syrup. “It’s during wintertime when there’s not a lot of other food available,” Luby says. “Bats are smart animals, and they come in and lick the sap stream. Occasionally, they are shedding the virus.” Luby’s team encouraged sap collectors to use skirts on trees to keep bats out of the sap stream. “We also went public with the data on the risks of date palm sap. That was very controversial initially because it was so closely connected to culture,” Luby says. “It’s kind of like telling the French that wine with dinner is a risk factor.” Ultimately, after the education campaign, Nipah cases declined.
‘We’re pushing beyond the carrying capacity of the planet. We are pushing into and exploiting more areas and exposing more people. There will be a SARS-CoV-3.’
During our restive truces with the viral world, we easily forget the unceasing mutations. While experts watched for Nipah and avian flu, coronaviruses schooled us in nature’s variability. Before SARS-CoV-1 broke out in 2003 with a 9 percent mortality rate, coronaviruses were known to cause only mild upper-respiratory infections. MERS followed in Saudi Arabia with a 35 percent mortality rate but, mercifully, a relatively low rate of transmission. “If the coronaviruses had just read our textbooks, they would have behaved better,” Luby says.
Whereas in previous centuries, outbreaks among humans often burned themselves out in remote villages, today’s coronaviruses jet around the globe. In late 2019, weeks after SARS-CoV-2 was detected in China, it turned up in California. “We’re pushing beyond the carrying capacity of the planet. We are pushing into and exploiting more areas and exposing more people, and we are also just so much more connected than we ever were,” Luby says. “There will be a SARS-CoV-3.”
Reservoir Hogs
Human expansion and its consequences are stirring further uncertainty into nature’s already formidable unpredictability. Global warming, habitat destruction, population growth, poverty and migrations—of both people and animals—are changing our relationships even with well-studied diseases. And what we know so far suggests that we are entering a new pathogenic frontier.
At first glance, the relationship between a population’s size and viral spread is straightforward. Viruses thrive in dense populations, where air, water, surfaces and so much else are shared. But while the idea of herd immunity through infection—rather than holding out for vaccines—may seem to be a viable solution, it doesn’t account for the fact that as viruses spread, they mutate. “The probability of that happening is a direct function of the number of people infected,” says Robert Siegel, ’76, MA ’77, MD ’90, a professor of microbiology and immunology. The larger that population, the greater the likelihood that a mutant will adapt to survive longer in the air or to better infect respiratory tracts, as we are seeing with SARS-CoV-2. The same is true for diseases spreading through large livestock populations crammed into limited spaces. Global increase in human population (on average, by 84 million annually) creates a chain reaction: Meat demand rises, more forests are razed, and more atmospheric carbon and methane are produced. Then, as the planet heats up and habitats vanish, wildlife and insects migrate, increasing the likelihood that even well-known diseases will become more devastating.
Consider Rift Valley Fever, a virus carried by mosquitoes and thought to have originated in bats. It has long infected cattle, sheep and people during rainy periods in East Africa, but in recent years, outbreaks have become more frequent and widespread. “When the rains come, you go from having zero mosquitoes to a million mosquitoes,” says Desiree LaBeaud, a professor of pediatrics specializing in infectious diseases and a senior fellow at the Woods Institute. “Climate change and more flooding events are leading to more outbreaks.”
Rift Valley fever hits livestock the hardest, causing nearly 100 percent of those pregnant to abort while killing 90 percent of the young and 10 percent of adults. For humans, typical consequences are fever, aches and dizziness, with small risks of vision loss, neurological damage or death. Twenty years ago, the disease spread beyond Africa through cattle trading, infecting both livestock and people on the border of Saudi Arabia and Yemen. Yet even as outbreaks grow larger and more frequent, there is little surveillance to prevent the disease from reaching the western hemisphere, which has hundreds of millions of cattle. “If the virus were to make it here, there’s a lot of potential for it to become endemic and to spread,” LaBeaud says.
The movement of millions of humans around the planet in conjunction with global warming has, in just the past few decades, caused known viruses to become newly established in the Americas. In 1999, West Nile virus—which originated in Africa—appeared in Queens, New York. In epidemiological lingo, the reservoir is the host species in which the virus multiplies, and the vector is the species that transmits the infection between organisms. For West Nile, both were present throughout the western hemisphere: Birds were the reservoirs and mosquitoes the vectors that transmitted the virus. The disease spread rapidly—especially along changing bird migratory routes—from Canada to Venezuela, infecting millions of people and killing thousands from encephalitis. Similarly, Chikungunya and Zika, both mosquito-borne viruses, have spread into the Americas and Europe.
Even long-established diseases such as yellow fever, dengue and malaria, which arrived in the western hemisphere during the slave trade, are expanding their ranges. Yellow fever—transmitted from nonhuman primates to humans via mosquitoes—found a new world replete with all three and caused deadly outbreaks across the Americas in the 18th and 19th centuries. In recent years, Brazil has experienced some of the worst flare-ups of yellow fever in nearly a century due to rapid deforestation that brings the mosquitoes down from the canopy and into impoverished settlements. “Most of the infected were young men working in the forest or along the edge,” says LaBeaud. “They’ll say, ‘Oh no, the monkeys are dropping dead out of the trees.’ They know that means yellow fever is around.”
To understand how diseases are spreading, LaBeaud partners with Erin Mordecai, an assistant professor of biology and a disease ecologist. Using LaBeaud’s field data, Mordecai models how climate change may redistribute mosquito-borne diseases. “You might think of it as the mosquito biting someone and picking up some blood and putting the pathogens in that blood into another person, but that’s not really the way it happens,” Mordecai says. “The pathogens in that blood meal have to avoid getting digested and excreted, so they have to be able to break through the mid-gut barrier of the mosquito and then replicate and disseminate throughout the body, and eventually bind to the salivary glands.” With rising temperatures, that process speeds up, as does the mosquito’s life cycle. Taking both into account, Mordecai’s modeling shows optimal temperatures for the spread of each disease: for dengue, 84 degrees; for malaria, a balmy 78. As average global temperatures rise, dengue could replace malaria across much of the world and spread as far north as Alaska and Scandinavia.
While less malaria sounds great, a corresponding increase in dengue is not a fair trade. For decades, public health measures have been developed to treat malaria and to target the Anopheles mosquito, which carries the pathogen. For example, Anopheles is nocturnal and can be killed with insecticide-treated bed nets. Aedes aegypti, which carries dengue, is diurnal. “One way to control malaria is to diagnose cases quickly and treat people with antimalarial drugs,” Mordecai says. “Well, the diagnostic test for malaria and the drugs that work against malaria don’t work for dengue.” In fact, no reliable treatment for dengue exists. The mortality rate of its severe form—though less than 1 percent with proper care—can be as high as 20 percent.
Living on the Edge
Historically, bats have had a bad rap in the West—nocturnal, diabolic, vampiric—even though they pollinate plants and keep insects in check. Though scientific data has yet to link them to the devil or living dead, they are host to, well, a host of pathogens, in part because of their proclivity for spending their days in conditions as crowded as house parties. (We’ve seen how that has worked out for humans with SARS-CoV-2.) “Bats are what viruses dream about at night,” Siegel quips—not just because of their population density and their roosting in excrement-filled caves, but also because of their ability to fly and disperse pathogens. They may also have immune systems perfectly calibrated to suppress viruses without eliminating them; or, through the high metabolic demands of mammalian flight, they may sufficiently raise their body temperatures at night to keep those pathogens in check, allowing for periods of latency and recrudescence (think herpes). These theories are unproven, but scientists are currently building cases. “Bat viruses adapted to fight a really immunologically adept host and then got a different host, like humans,” Siegel says. “They don’t realize that they’ve got a weakling for a host, basically, so we suffer the consequences.”
‘People assume that we have to fear wildlife, but actually wildlife has as much if not more to fear from us.’
Though bats hardly rise to mascot status for humans, humans are truly the stuff of nightmares for bats—not to mention other species. We’ve contributed to atmospheric carbon levels that are consistently higher than any time in the past 3 million to 4 million years, and global temperatures are soaring. The natural world—and by that, we’re talking ecological systems so complex and vast that scientists have barely tapped their mysteries—is buckling under the strain. Less obvious is the fact that sometimes we are driving the spread of diseases. Professor Elizabeth Hadly, an environmental biologist and a senior fellow at the Woods Institute, studied bats in Costa Rica, where farming has fragmented forests. Blood tests showed that 33 percent of them carried bartonella, a bacterium implicated in cat scratch fever, among other conditions, in humans. While this prevalence was remarkable, Hadly says, the real surprise came when her lab built a phylogenetic tree of every known sample of bartonella collected in the world, showing the many species affected. Human activity appeared to be spreading independently evolved strains of the bacterium into new regions and between species, with evidence of transmission from domesticated animals to bats. “Many people assume that we have to fear wildlife,” Hadly says, “but actually wildlife has as much if not more to fear from us.”
This risk of spillover—both to and from humans—increases with climate change, which continually shifts the natural environments of animals toward the poles. A changing climate can cause flowers to bloom and insects to hatch at different times, and animals that have adapted to year-round food sources suddenly face privation. “As we all know,” Hadly says, “when you’re stressed, it’s pretty common to get sick, because stress basically causes a lot of wear and tear on your system.” Starving bats on frantic forays into human farmland are at higher risk of being contagious.

Hadly evokes the iconic image of an orangutan in a single tree, surrounded by clear-cut forest. We have become accustomed to such images of charismatic, keystone species: the polar bear trapped on the ice floe. But what we fail to see, Hadly says, is just how many wildlife populations are locked within increasingly fragmented landscapes. This not only disrupts migratory patterns and creates more edges where humans and animals come into contact, but it also prevents animals from finding new homes as the planet warms, since entire regions are now denuded. “How are they going to get across that area?” Hadly asks. “They end up either just dying or kind of piling up on the last place they can persist—and that is exactly where human domination of the landscape begins.” Bats that had inhabited the same caves for thousands of years suddenly begin roosting in the attics of homes and barns.
Climate change essentially turns these edges into a paradise for pathogens: large numbers of humans, livestock and wildlife crammed together, sharing water, air and nutrients, contaminating one another with fecal matter. A virus can jump to a domesticated animal when a sick bat feeds from a trough or gets caught in the jaws of a dog or cat. From there, millions of humans and other animals are easily within reach. By one estimate, 1.7 million viruses have yet to be discovered in mammals and birds, of which 800,000 might be transmissible to humans. And we have little understanding of how they affect the wildlife that carry them. “We don’t know the basics of how bats or other mammals are responding to the waxing and waning of diseases,” Hadly says.
While animals are forced to infiltrate human territory, our own most vulnerable are the ones on the front lines of diseases. Americans have seen this play out with many service industry workers during COVID-19. Those with limited access to health care and who live in crowded conditions are at greater risk. Their increased vulnerability can give a pathogen the foothold it needs to begin to spread, says James Jones, an associate professor of earth system science and a senior fellow at the Woods Institute. Furthermore, in many countries, rapid urbanization leaves city dwellers with nostalgia for village life and an appetite for wild meats from home. And in rural settings, poor people—living at the human-wild interface with less and less buffer between them and natural habitats—find themselves foraging where humans once rarely ventured, says Laura Bloomfield, ’07, MS ’10, PhD ’20. “You have these islands of forest, which have been diminishing over time. People have higher access to the core habitat at the center of that forest,” she says. Her research in Uganda showed that people living in these regions had a greater risk of contact with nonhuman primates even in the absence of hunting. Though additional forest may be cleared as local farms suffer the effects of climate change, the growing global demand for timber, sugar, palm oil and other exports is at the core of the problem, says Eric Lambin, a professor of earth system science and a senior fellow at the Woods Institute.
The simplistic version of the COVID-19 tale is that a bat flapped out of a cave and happened to infect an intermediary animal, which ended up in a market. But the complex pandemic reality is that as humans have reshaped the earth to our needs, desperate and vulnerable animals, sometimes carrying disease, are finding what may be their final refuge at the edge of human habitats—among our own most desperate and vulnerable.
Is There Hope?
Fevers. Blindness. Hemorrhaging. Inflamed brains. And now a global pandemic, which—while not the most lethal one imaginable—has devastated communities and left us hankering for good news. And there is some. The Coalition for Epidemic Preparedness Innovations (CEPI) is developing seven high-priority vaccines: Nipah, Rift Valley fever, Chikungunya, Ebola, Lassa (for a virus from rats), MERS (which, alongside Ebola, helped pave the way for the rapid creation of the SARS-CoV-2 vaccine) and Disease X—which is not a vaccine, per se, but a platform from which future vaccines could be developed.
Among COVID’s lessons is the importance of developing treatments for viral infection, to save lives until vaccines are created and distributed. Jan Carette, a professor of microbiology and immunology, is working to create broad-spectrum antiviral medicines, not unlike certain antibiotics. He does this by focusing on how viruses use animal cells to replicate. Rather than target the virus itself, he blocks the cellular proteins that the virus needs to make a copy of itself, keeping a lid on viral load in the infected body and buying hosts—us—time to kick the disease. “What host components does the virus latch onto in order to start a successful infection?” Carette says. His team has already identified a protein used by flaviviruses (yellow fever, dengue and Zika) and a drug that inhibits them, as well as a protein that, once neutralized in mice, completely protects them from enteroviruses (those that cause polio, some forms of the common cold and more). He is currently evaluating the safety of treatment and the best drugs to use.
But many of the most effective measures against pandemics lie in governance—from addressing people’s basic needs to funding the virological sleuthing that detects foes measured in nanometers. Michele Barry, senior associate dean of global health at Stanford Medicine and director of the Center for Innovation in Global Health, co-authored a 2020 paper on how improving rural health care in Borneo decreased illegal logging, since many of the people logging did so to pay for medical expenses. One of her students, Isabel Jones, PhD ’20, “did a deep dive and what we called ‘radical listening’ to hear what people wanted that would prevent them from logging,” Barry says. “And what they wanted was health care.” Ten years after a medical clinic was established, illegal logging had decreased by 70 percent and better access to health care had reduced the rates of infectious diseases.
‘If 40 percent of the population think the virus is a hoax and another 20 percent think it’s actually the harbinger of a new world government coming to put mind-control chips in your brain, your optimal strategies won’t do a damn bit of good.’
Barry believes that governments must provide better funding for the WHO, CEPI and PREDICT, a USAID program that identified 1,200 viruses capable of infecting humans, among them more than 160 previously unknown coronaviruses. (PREDICT, part of USAID’s Emerging Pandemic Threats program, was defunded in 2019.) “When we look at the WHO, its budget is not even as much as the Stanford Hospital budget,” Barry says, “and you’re talking about the budget for the entire world.” Her goal is to establish a center for planetary health at Stanford, since ecosystem health is inseparable from human health, just as the health of other nations is inseparable from that of our own. Barry believes we need to put some of our focus on other countries, or “it’s hopeless for pandemics—unless we work in a global fashion.”
The challenge, of course, is that political—and corporate—leadership changes, often reversing previously established initiatives. But some entrepreneurs are devising ways to mitigate pandemics by writing them into the business model. The virologist Nathan Wolfe, ’92, who describes his former work as a virus hunter in The Viral Storm: The Dawn of a New Pandemic Age, has added pandemics to the list of natural disasters against which companies should insure themselves. Just as hurricane or earthquake insurance requires that policyholders meet standards and take precautions, pandemic insurance obliges businesses to be prepared. “To qualify for the insurance policy,” Wolfe says, “you have to show that you have reasonable surveillance, and you have to have contingency plans. You are incentivized to look for [virus outbreaks] because if you see cases, you know that the certification of those cases will lead to the release of funds that permit you to control the outbreak early.”
But companies showed virtually no interest in pandemic insurance before COVID-19, and the cause may lie in how humans reason: We don’t worry about problems that don’t regularly arise. “When public health works, we don’t see illness and disease, right?” says James Jones. “People aren’t able to make that counter-factual scenario, where if we didn’t have the public health, what would this look like?” For Jones, understanding human behavior is crucial to preventing pandemics. “If 40 percent of the population think the virus is a hoax and another 20 percent think it’s actually the harbinger of a new world government coming to put mind-control chips in your brain, your optimal strategies won’t do a damn bit of good.”
Behavioral response is crucial even at the most basic level, such as perceiving a disease as harmless and ignoring public health orders. “That’s the paradox of COVID,” Jones says. “Because it, for the most part, is a mild disease and most people who are infected will recover, people don’t take it as seriously as something like Ebola.” He recently received a National Science Foundation grant to investigate how ideas about pandemics emerge, how they influence transmission and how they can be overcome. Understanding human belief might prove key to encouraging people not only to adopt preventive measures and get vaccinated, but also to run pandemic-conscious companies and elect governments that invest in surveillance, prevention and treatment.
As for the beliefs of government leaders, those most attuned to pandemic prevention are in places that have experienced previous outbreaks. “These are real-world ‘simulations’ that countries have gone through,” Maria Van Kerkhove says. “Each time, they learn and they adapt and they adjust.” For instance, in 2015, a single individual who had visited several countries in the Middle East returned home to South Korea and started a MERS outbreak with 186 cases and 38 deaths. “The country had more than 70,000 people quarantined at one point,” she says. “The economic impact was on the order of $8 billion.” That experience with MERS made South Korea more responsive to COVID-19 than many other countries.
But even nations with comparatively few resources—Nigeria, Senegal and Rwanda—have successfully mobilized public health staff experienced with outbreaks. “Countries across Asia and across Africa know the value of basic public health measures. This is Epidemiology 101,” Van Kerkhove says. “You build the system from the ground up. You have the workforce in place to find cases and do cluster investigations and have community health workers go door-to-door. These countries may not have the most robust hospital system or the most sophisticated lab system, but every single one of them knows how to use the resources they have strategically.” Van Kerkhove hopes that in many countries—and especially in those of North America and Europe, where quality of individual care is emphasized over public health—the experience of COVID-19 results in better systems. And each nation, she believes, will have to take into consideration many larger factors—people and animals migrating and the disruption of ecosystems. “We have an opportunity here to use this horrible experience that we’ve all gone through to better ourselves and better the world we live in and the world we’re giving to our children and our children’s children,” she says. “This is no longer theoretical. It’s real.”
Deni Ellis Béchard is a senior writer at Stanford. Email him at dbechard@stanford.edu.