Published: 07/24/2020
Dear Global Health Colleagues,
Day by day, we gain a deeper understanding of the pathology of COVID-19 and how we can control the spread of the virus. In PubMed alone, we are seeing roughly 2,000 peer-reviewed articles per week. And yet, observing the state of the pandemic, this understanding appears to be unrelated to our global ability to coordinate around an effective response.
The United States exemplifies the potential disparity between knowledge and governance. On July 15th, hospitals were mandated to report daily coronavirus case information not to the Centers for Disease Control, which has been charged with collecting data of this nature for the past 15 years, but rather exclusively to the Department of Health and Human Services, an abrupt decision that is drawing much criticism and scrutiny as a potential threat to accurate public information about the state of the crisis.
This, combined with the United States formal intent to withdraw from the World Health Organization on July 7th implies a larger reshaping of the US’s approach to global health governance. This is the subject of our upcoming webinar this Friday, which we hope you will join us for.
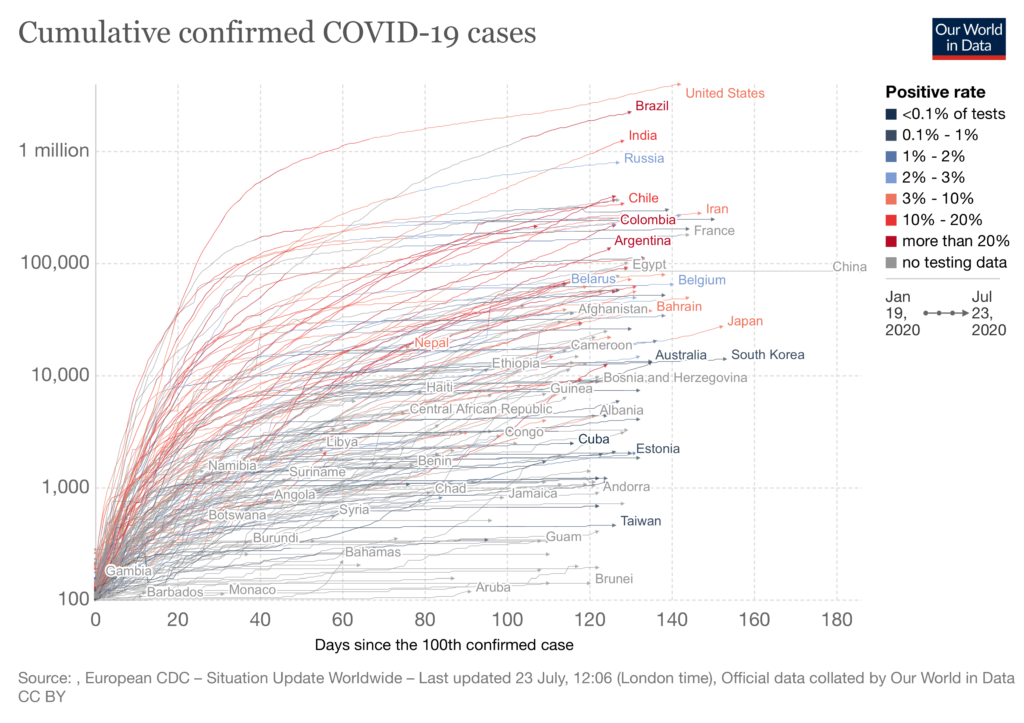
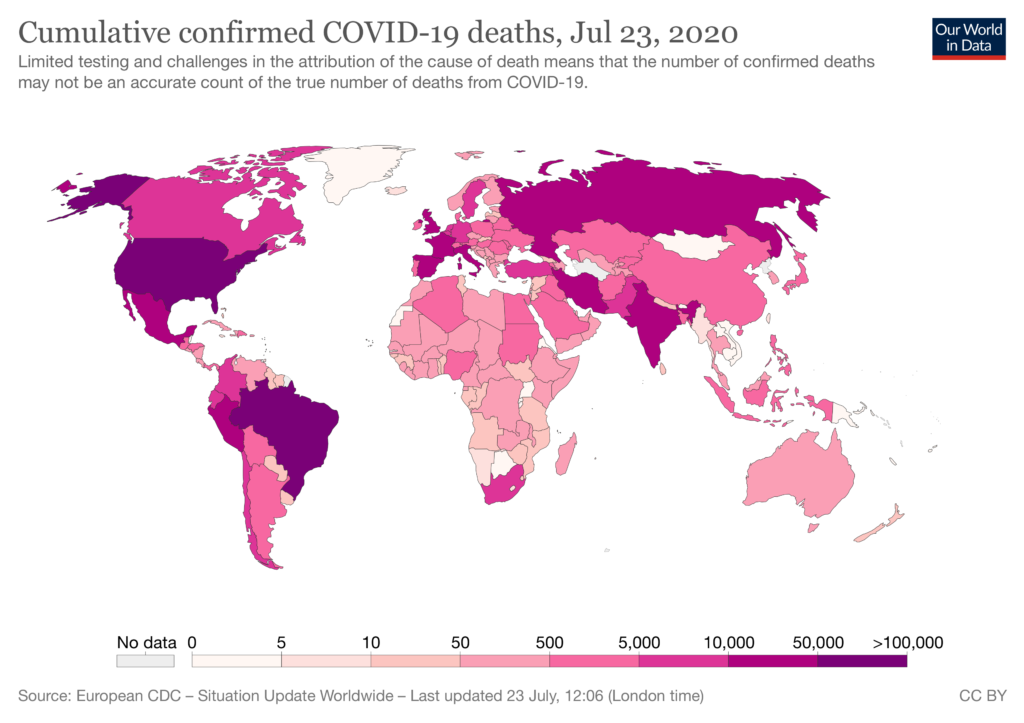
We continue to see a rise in cases around the world, and we are particularly concerned about South America and Africa. While the continent of Africa had initially maintained low-levels of disease, the recent surges in South Africa, Kenya, Zambia and Namibia are alarming. We are also reminded by stories like the one below from my friend in Australia, that extreme vigilance is required in order to maintain any gains of low levels of community transmission.
That said, there is progress on the tool development front. We have early and promising therapeutic and vaccine results, and there is progress towards a point-of-care diagnostic. All tools would be game-changers. In addition to several insightful articles below about the global impact of COVID-19 on marginalized groups, I am also proud to highlight fantastic work produced by four of Stanford Global Health’s Faculty Fellows.
We may not be able to claim pride in our coordinated effort against COVID-19, but we can report a greater understanding of the virus’s many effects on society and interactions with other ongoing trends, evidenced in many of the articles below.
In solidarity,
Michele Barry
Drs. Ben and A. Jess Shenson Professor of Medicine and Tropical Diseases
Director of the Center for Innovation in Global Health
Senior Associate Dean for Global Health, Stanford University
Resources
Global Trends and Topics
- COVID-19 and the dangers of Sinophobia (7/18/20): Important commentary in the Lancet on how growing political rifts between China and the West are increasing Sinophobia at a time when the world is much indebted to the medical community of mainland China and Hong Kong.
- The Climate Crisis and Covid-19 — A Major Threat to the Pandemic Response (7/15/20): Climate and health have always been linked, but now the effects of this largely ignored relationship are unfurling before our eyes and revealing critical weaknesses for future resilience.
- Serious violations of health workers’ rights during pandemic (7/14/20): This editorial draws on a startling Amnesty International report on the growing stigmatization and violence against healthcare workers around the world.
- Unequal effects of the COVID-19 pandemic on scientists (7/15/20): Drawing on survey results of 4,535 researchers in the US and Europe, this paper highlights how women suffer a greater impact on their work and careers.
Regional News
- Lessons from the Ebola epidemics and their applications for COVID‐19 pandemic response in sub‐Saharan Africa (7/12/20): This article draws upon the differences and similarities between the Ebola epidemic and COVID-19 pandemic in Sub-Saharan Africa, deriving lessons and recommendations on how to translate these learnings to present day preparedness.
- COVID-19 in Yemen: a crisis within crises (7/11/20): This commentary provides a startling overview of Yemen’s probable coming nexus of maladies: continued war, massively re-emerged communicable diseases, and COVID-19. It is a dire situation that demands attention.
- Exploring the Impact of COVID-19 on the Sustainability of Health Critical Care Systems in South America (7/5/20): Aimed at addressing “the gap in the analysis of the incidence of COVID-19 in six South American countries”, this paper paints a picture of a drastically underprepared continent housing a rapidly evolving epicenter.
Underserved Populations and Health Disparities
- LGBTIQ community faces new challenges during COVID-19 (7/14/20): A UN field story on the COVID-19 vulnerabilities faced by LGBTIQ community in Myanmar, as well as their admirable and bold efforts to combat the virus.
- Haitian mental health needs rise yet again with COVID-19 trauma (7/17/20): In a nation plagued by severe trauma, COVID-19 is contributing to the great need for mental health services.
Notes from the Field

Dr. Karin Leder
Professor of Infectious Disease Epidemiology in the School of Public Health and Preventive Medicine at Monash University
As of July 7th, Melbournians are back in lockdown. A few weeks prior, we were counting the days until restrictions were sequentially lifted. Instead, we find ourselves back in the position we were in in March — allowed to leave home only for work, healthcare, exercise or buying essentials.
Six weeks ago many Melbournians were feeling optimistic and relieved. In early June, Victoria had a day with zero recorded new cases of COVID-19. For two months, Australia had case counts of less than 30 per day, nationally. Daily new case numbers were so low that almost every new case made the news. Almost every non-imported case was assigned an outbreak contact-tracing team. We were in an enviable position.
Inevitably, cases would continue to occur as long as we repatriated individuals from overseas. Appropriate public health measures were taken: initially home quarantine for all overseas arrivals, border closure to all non-citizens and non-residents, and then, on March 27th, mandatory hotel quarantine for overseas arrivals. The logistics required to organize quarantining in hotels for the hundreds of people arriving daily needed to be coordinated literally overnight.
Victoria enlisted private security firms to guard the travelers coming into hotels, thus using people with minimal training and experience for a public health job in a high-risk setting. Two hotel-associated outbreaks emerged, affecting hotel staff and particularly security guards, who then spread COVID-19 to their often large families and beyond—into other workplaces, schools, and the larger community.
We cannot be sure if this is the entire explanation for the recent flare in Victorian cases, which reached its highest peak with 484 cases on July 22nd. This didn’t happen in other states which also received overseas visitors. Perhaps there was an element of luck involved. Perhaps a contributing factor was that other states used police and Australian Defense Force personnel as well as security contractors to assist with their hotel quarantining. But rumors suggest that some security guards let those in quarantine go out shopping, mingle with other hotel inhabitants, and possibly even engaged in sexual contact with travelers while in isolation—an avoidable factor, if true. A judicial inquiry is currently underway.
Australia has differed from many other countries by disallowing lifting of restrictions until essentially complete control of community transmission has been achieved. Most states and territories have reached virtual elimination — a success well beyond our initial expectations. To get to this point, we have paid a high economic price, with many believing our shutdowns were disproportionate to case numbers and overly drastic. Failure in Melbourne due to the mismanagement of obvious ongoing source (returned travelers) has provoked anger and frustration.
Now Melbournians must accept being back in lockdown and are facing the prospect of heightened restrictions. The questions yet to be answered are how well this will be tolerated, and how long it will take second time round to flatten the curve.

Upcoming Events and Lectures
The Role of the WHO and the Risks of US Withdrawal
Friday July 24, 2020 | 9:30am PSTStanford Center for Innovation in Global Health, Stanford University
Event information and registration.
On July 7, the Trump administration submitted formal notice of its intent to withdraw the United States from the World Health Organization. This decision was made in the midst of the largest public health crisis in over a century, a time of critical need for a global governing body to coordinate all stakeholders around a response to the COVID-19 pandemic. In this panel, led by Dr. Michele Barry, Director of the Center for Innovation in Global Health, experts will present the important role of the WHO in providing global health governance and in supporting low-and-middle income countries, as well as discuss the risks and ramifications of this decision.
The Health Crisis on the Northern Mexico Border: Cross-Border Implications of US Immigration Policies
Tuesday, July 28th | 10:00am – 11:30am ET
Harvard Global Health Institute
Event information and registration.
This webinar brings together experts in immigration policy and public health to discuss the growing health crisis on the border. Panelists will discuss the most pressing health needs of this population; how policies and practices in the U.S. and Mexico are exacerbating health risks of migrants; and what action is needed to protect them. Each panelist brings a unique perspective, and will add context to the challenges facing asylum seekers, as well as those who care for them, during this global crisis.
COVID-19: The Impact in Latin America
Wednesday, August 5, 2020 | 12:00pm PST
King Center on Global Development with the Stanford Center for Latin American Studies
Event information and registration.
As COVID-19 cases rise across Latin America, countries have taken different approaches to curb the spread of the virus with varying degrees of effectiveness. During this panel discussion, leading experts will analyze the impacts of the pandemic on health, social protection, and the economy in countries across Latin America, as well as provide a data‐driven assessment of how countries have responded.
New Funding Opportunities Specific to COVID-19
COVID Catalyst Pop-Up
Available to Stanford researchers only. This RFA is a funded effort supported by the leadership of Stanford Medicine to identify and implement COVID-inspired innovations coming from within the Stanford community. Selected projects will receive funding, implementation support, business planning, and regulatory navigation.
View here.
Online List of COVID-19 Research Opportunities
Stanford’s Research Management Group has created a website that provides a complete listing of funding opportunities for COVID-19 research. The site also provides sponsor and University guidance on grants, clinical trials, and award management impacted by COVID-19. See funding opportunities.
CIGH Faculty Fellow’s Global Research on COVID-19
The Contribution of the Age Distribution of Cases to COVID-19 Case Fatality Across Countries(7/22/19) : Stanford Global Health’s Faculty Fellow Dr. Pascal Geldsetzer co-authored this article seeking to measure the contribution of distortions from the age distributions of confirmed cases to CFRs within and across populations.
Digital COVID-19 Training for Healthcare Workers : Created in collaboration with Stanford Emergency Medicine International, this digitalMEdic resource creates equitable access to online medical trainings.
Pulse oximetry in low-resource settings during the COVID-19 pandemic (7/3/19) : Stanford Global Health’s Faculty Fellow Dr. Tom Weiser on the distribution of essential respiratory monitoring equipment in Ethiopia and other low-resource settings during the COVID-19 pandemic.
Stanford works with California prisons to test and prevent COVID-19 (6/16/20) : Stanford Global Health’s Faculty Fellow Dr. Jason Andrews partners with other researchers to accelerate the much-needed response to COVID-19 in California prisons.